Brain networks, seizures and epilepsy surgery
A new perspective of the brain
The 21st century is the era of networks. You are probably familiar with many examples of networks: the power grid network, the map of road or railway connections or even your social contacts. We can also use networks to describe our brains. These can be built from the connections — called synapses — between neurons, but with over a hundred billion neurons and a trillion synapses in the human brain, such a description is not possible for the whole brain. For this reason we often divide the brain in different regions, usually some tens or hundreds of them. These areas can be identified on the basis of anatomy, a specific function, or a specific connectivity profile. For instance, certain areas can be involved in vision (the visual cortex) or language (Broca areas).
To construct a network, we need to then measure how the different regions interact with each other. In brain networks, two types of interactions are usually recorded: physical interactions, meaning that there is a physical path connecting the two regions, or functional interactions, meaning that the activity of the two regions is related. Structural connections can be observed with MRI (Magnetic Resonance Imaging) techniques, and functional ones with EEG (Electro-EncephaloGram), MEG (Magneto-EncephaloGram) or fMRI (functional MRI).
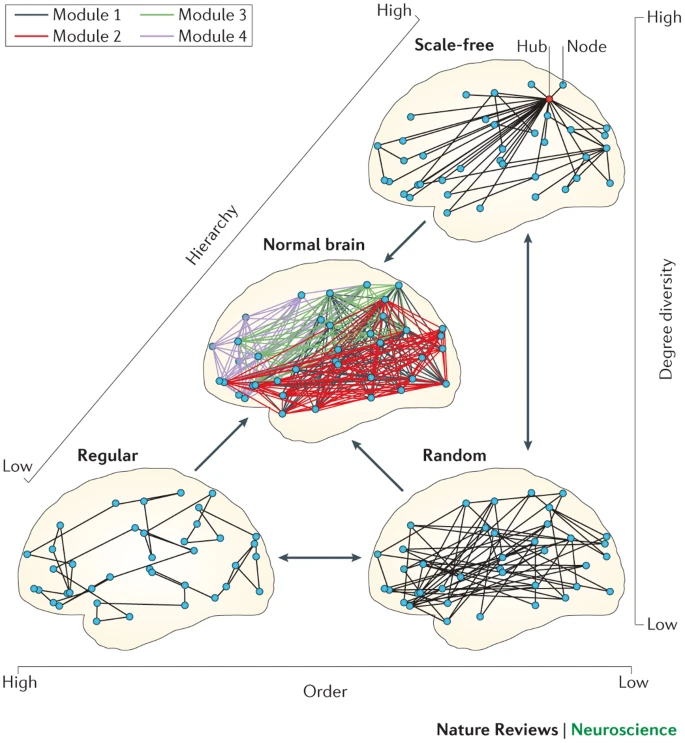
Brain networks, as well as other types of complex networks, have certain characteristics. A very relevant property in many networks is the presence of hubs: these are regions that play a central role in the network. They are usually very well connected, which means that they can transmit information very quickly to other regions. In a railway network, for instance, the hub is the central station that has trains (connections) to all other large stations. In a friendship network, a hub is a popular person who knows many other (important) people. The same notion applies to the brain, where hubs are very important for brain function.
We can use the network description of the brain to study its properties. Once the properties of a healthy brain are well known, we can look at how different brain disorders affect the brain network. Maybe some roads disappear, or maybe some hubs loose their importance. We can use this knowledge to understand brain disorders better and, eventually, to treat them better.
Figure reproduced from (CJ Stam, Nature Reviews Neuroscience, 2014) with permission from the author.
Epilepsy and epilepsy surgery: the epileptogenic zone
Epilepsy is a common neurological disorder that causes frequent seizures: busts of electrical activity in the brain that disrupt normal function. Seizures can present in many forms, and the recurrent occurrence of debilitating seizures can pose a large burden in the quality of life. There is no one single cause of epilepsy, which can occur at any age. Seizures can appear as a consequence of a brain tumor, structural abnormalities on the brain, or a chemical imbalance, for instance.
Seizures are initially treated with anti-epileptic drugs. However, for about one third of the people affected with epilepsy, medication does not prove to be effective enough to stop the seizures. They are then said to have refractory epilepsy. But even then there are still options, such as transcranial stimulation to try to prevent seizures or epilepsy surgery.
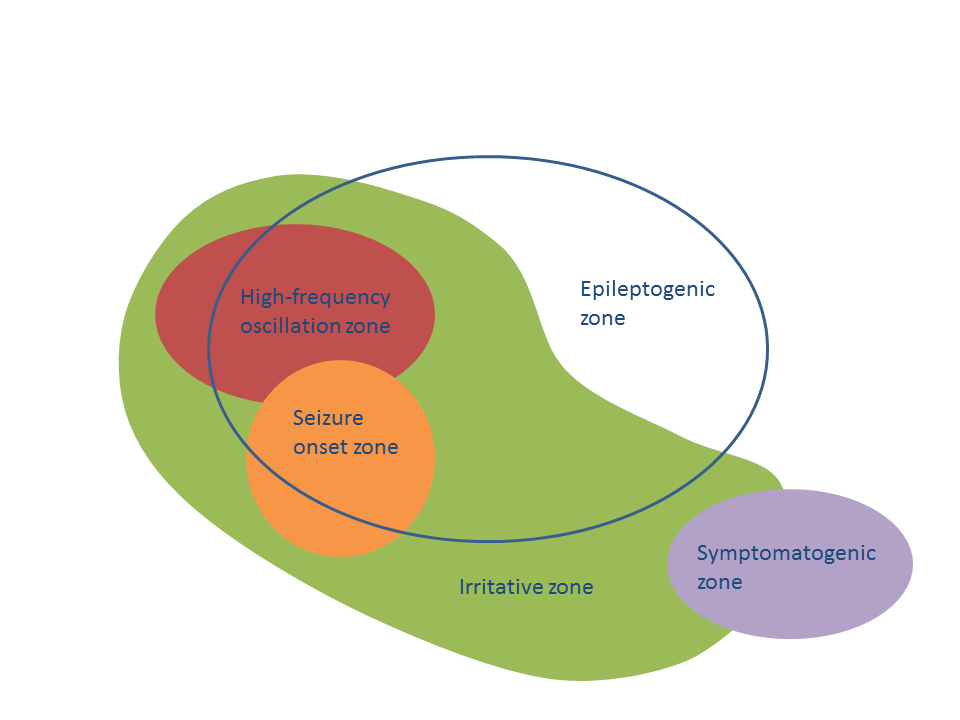
Epilepsy surgery is currently the treatment of choice for people with refractory epilepsy. Its aim is simple: removing the minimal amount of brain tissue to that seizures stop. This is known as the Epileptogenic Zone (EZ). However, there is a deep problem hiding behind this definition: whether the EZ was found or not — whether the surgery is successful or not — can only be known after the surgery has taken place. Thus, before performing the surgery, we want to be very sure that it will help the patient. For this, a large battery of presurgical tests is carried out. These include functional and structural Magnetic Resonance Imaging (MRI), ElectroEncephalogram scans (EEG) and Magnetoencephalogram scans (MEG). These tests are not invasive, and often times they are enough to determine if the patient should have surgery. If the information is conflicting, or not enough, an invasive test is carried out to directly measure brain activity on the relevant brain areas by placing electrodes inside the brain tissue.
All these tests aim at finding where the seizures are starting — known as the Seizure Onset Zone (SOZ) and how they propagate thereafter. In order for the surgery to go through, there are several pre-requisites. First, the presurgical tests must succeed in identifying an hypothesis for the SOZ. Second, this should be localized in one relatively small brain region. Third, this region must be operable: not all regions in the brain can be removed safely. If all these requisites are fulfilled, then the clinical team comes up with a surgical plan to perform the resection.
Despite all the careful presurgical planning, about one third of the patients who undergo epilepsy surgery continue to have seizures afterwards (although often with a reduced seizure burden, that is, with fewer or less severe seizures). Currently, several research teams across the world — including us at Amsterdam UMC — are working to improve this number. This research makes use of the most recent developments on network theory and computer simulations.